Case Studies and Homeopathy Treatment
Case of Rosaceae
Name : Ms. N. B. Age : 27 years Eduacation : MSc Applied Economics + completing B Ed for prior formalities. Currently training to be a professional Hatha Yoga Teacher. Occupation Left the previous job due to excess job pressure. Chief Complaint : Face : Macular patches on the cheek and forehead since few months. A/F : stress. Sun agg+++ No itching or burning. Only hyperpigmentation: redness of cheeks, upper (bridge of the nose) and forehead. Life Situation and Mind : In patient’s language : - I on the other hand have been at the receiving end of the unhappy marriage my parents have had throughout, and continue to be caught between their marital discord. I am much closer to my mother than father; my father and I share a very disturbed relationship and hence, I maintain my distance. As supportive as my mother is towards me, I have been subject to a lot of emotional dumping and have been forced to grow up too soon. I have started to make and be very firm in terms of my boundaries now as I have understood the kind of impact my family has had and continues to have on my mental health. - My childhood trauma does have a way of showing up from time to time – a child growing up in an unhappy house does in many occasions result in an adult who can be unhappy. I have experienced this and am still exposed to unhappy home circumstances but it is not nearly as bad as it used to be. I have greatly started to work on my mental health and that has brought me a certain amount of peace. - I do not have any financial responsibilities currently. I quit my job due to supremely high stress levels and thus do not have an income as of now. That does not bother me as much as it used to as my mother is very supportive of my dream to become a professional Yoga teacher.
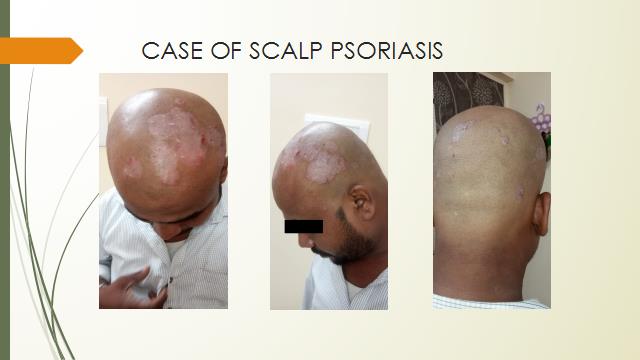
A Case of Scalp Psoriasis
Preliminary Data- Name- Mr. P. S. Chief Complaints- Skin macuplopapular Eruption- since 4 months Onset with scalp followed by medial aspect of the thighs left to right, then knees , back and then arms. Earlier Small eruptions increasing in size. Itching++ followed by bleeding from the eruptions of the back. Started with allopathic Rx 9 days ago. Earlier applied Clobestol+Salicylic Acid + Coal Tar cream - that caused eruptions on the scalp- small papular erutions- with black pigmentation
A CASE OF PSORIASIS
Name : Mrs. M. K. Age : 40 years Occupation : House Wife Chief Complaint : Raised papular eruptions on the legs : from feet to the mid leg and radiating upwards. Scaling of the skin++ with skin dryness Intense itching+++, hyper pigmentation black discolouration of the skin with hypopigmentation in the centre of the patches. Burning sensation scratching It has been a chronic complain since many years - Occasional headache due to loss of sleep s/b skin specialist diagnosed as Psoriasis Patient as a person : constantly worrying and anxiety even while narrating symptoms Obese App : Good Desires : Spicy++ Sleep: disturbed, due to domestic chores. Has to get up early morning at 4 am to fill water Stool : NAD Menstrual history : scanty . 23 days backache ++ Leucorrhoea intermittently Obs History 1 ftnd girl Family History : Mother : OA Knees Diabetes Father- : HTN Elder Sister : Asthma Younger sister : NAD, youngest brother : Asthma Nature : Variable. Sometimes weeps easily. Irritability+++ consolation Stays with her daughter and a husband on rented house. She has studied up to X std. Stressed of husband have habit of alcohol drinking and Tobacco chewing, having financial constraints.
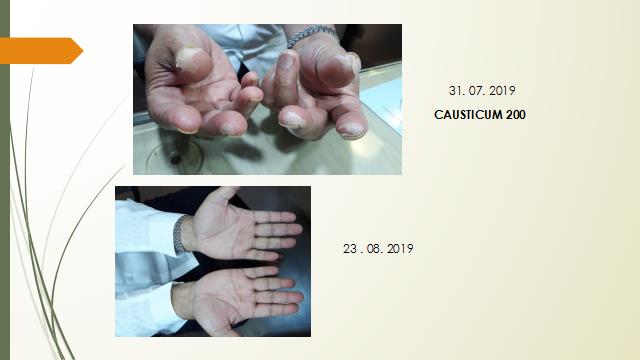
Case of PALMO PLANTAR PSORIASIS
Preliminary Data- Name- Mr. R. V. Age- 78 years Occupation- MD of a Chemical and Perfumeries Company. K/C/O- Diabetes Mellitus since 10 years. Dyslipidemia and HTN since 12 years. Taking medications for the same. Chief Complaints – 1. Peeling of skin - since 3 months onset- dryness sensation after 8-10 days, then skin starts peeling. Generalities – Desires- Prawns+++, fish++, seafood Thermally- Ambithermal towards Chilly. Thirst- less Mentals– Industrious+++ Disputes in the family. Had to give a huge amount of money to relatives. Patient said I can tolerate murders but not injustice. Patient started crying. Fault finding. Critical. Angry+++ Daughter says he does not talk so much generally. Likes to sit alone. CRIES EASILY
Case Seborrheic Dermatitis
Name- Baby. S M. Sex : Female Age- 2 years 2 months. Wt- 11.2 kgs Ht- 87cms C/ O : 1. Hair scalp- Itching and scaling of the scalp since few months 2. Recurrent Colds and cough A/F- Cold foods and drinks, ice creams, cold draft of air. But desires cold. Since 6 months of birth. Runny nose- thin watery. With cough rattling. Frequency every 15-20 days. Physical generals : Stools : Constipation. Dry and Hard stools. Does not cry but has to strain. No flatulence. Offensive and dark brown. Perspiration : frontal and temporal above the ears. Desires- savories, Cold+++ Thermally Hot Birth History – FTND, Physiological Jaundice at birth. Mind – Playful. Shares her toys. Does not stay alone in darkness.
A case of Eczema
A 35 year old Dr. A. visited us for her skin complaints. The complaints had started since 3 months on the face. Papular eruptions around the mouth were itching ++ and burning washing sun exposure. She had a dry patch on the left eye lid- which had scaling and itching patting the skin dry. She was applying topical steroid ointment and taking oral steroids. Associated complaints of Migraine: throbbing headache – forehead and occipital aggravation sun+++. This complaint has been bothering her since the past 11 years. Occasional episodes of vomiting during headache. Takes diclofenac injections when pain is unbearable. Generalities: desires – spicy 2+. Aversion : sweets++. Thermally : Ambithermal. Aversion to sun +++, photo sensitivity. Sleep is good Patient is a mother of 3 children - 9 years (Male, LSCS), 7 years (Male, LSCS) and 2 years (Male, LSCS). Menstrual history was normal. No significant Past History. F/H : Mother – ILD (deceased), Father- H/O Fall (deceased), 5 sisters ( Eldest- ILD, Younger- ILD, rest- NAD, 6Brothers (Eldest- ILD).
Case of Atopic Dermatitis
Name: Baby A. N. Sex: Female Age/DOB: 4 years., C/O : Skin- White hypo-pigmented patches - Right arm, shoulder, legs. Onset with small circular pigmentation and redness Itching aggravation after bathing Red papular eruptions on thighs – Itching++ Physical Generals : Sometimes talks in sleep, Dreams a bit. Grinding of teeth whenever she in angry (but nothing in sleep). Right side sleep position (initial) Stools : Constipation- alternate days passes stool. Dry. Chilly Birth History : Normal delivery with Vacuum (epidural). Wt- 3.4kgs. Milestones on time. Mind : She gets easily angry and cranky , possibly triggered by hunger or tiredness- especially when she is refused something like watching the phone, etc. Irritable when hungry. She is a little reserved and shy while talking to new people or even while making new friends. (got feedback from school). Very good and highly inclined towards art/ crafts, etc. loves to have conversations. Curious. Likes to be read to. Picks up stories and characters and builds up on them well.
Case of Hand and Feet Eczema
On the 5th of March'19, a 4-month-old baby S., was brought to us by her mother with the complaint of blisters and pustular eruptions spread extensively on the body. Redness and swelling of the feet and hands were seen. . The complaints had started in last month of 2018. The eruptions appeared as small vesicles on the abdomen, back, upper and lower extremities and then extended to the scalp. She was admitted in the hospital for 3 days for her acute respiratory complaints, after which the skin complaints had slightly reduced and then reappeared severely. It progressed as pustular eruptions from the webs of toes and feet to the hands. The nails were discolored. Mother's history during pregnancy revealed that she had Gestational Diabetes and was on the medications throughout her pregnancy. She also mentioned that she was under a lot of stress due to family issues with her in-laws. The father worked on the ship, so he was seldom around. The patient's generals were normal. P/H: of recurrent cold and cough when the weather changes. Based on the repertorisation we choose Dulcamara 200, 2 doses were given in a week. Later on, as the case and complaints evolved further on 12th March'19, Merc Sol 30 (1 dose) was given for her itching and increase in the number of pustular eruptions on the scalp. She responded very well within 2 weeks, the eruptions started drying and size of the blisters started reducing, no new eruptions or blisters were seen and the itching had reduced considerably. It was then repeated infrequently. A deep acting remedy was introduced. – SULPHUR 30 to complete the process of total healing.
A Case of Smoker’s Bronchitis
A 64/M, Mr. C. D., a chronic smoker was complaining of severe breathlessness on sitting and dry cough. On Examination chest had rhonchi++. Recent history of angioplasty in Jan 2019 with severe occlusion in LCX artery. Bloating of the abdomen++ Rx : Spongia Tosta 200 05/08/2019 Cough was better after 3 weeks, but Cough aggravation again due to inhalation of fumes Bloating of abdomen. Old complaint of lumbago. Rx : Lycopodium 200 weekly 19/09/2019 Cough better difficult expectoration. Occasional Bloating of abdomen+ with flatulence. Rx : Lycopodium 200 weekly. Over a period of 3 months, he had less episodes of severe cough and breathlessness. Since he could not leave smoking completely, due to maintaining cause of smoking results were inconsistent but still better compare to past episodes.
Elderly lady with COPD
A 71/F, Mrs. A. M., K/C/O of HTN & long standing Bronchial Asthma and now progressed to a COPD. She was complaining of cold and cough which has been lingering since weeks after and acute attack. Cough- whitish, sometimes easily. Cannot bear Cold draft of air. Complaints aggravations monsoons, worse cold foods. She has been taking inhaler since many years. Pain in the abdomen > passing flatus. Sleep is hardly for 5/6 hours on the right side. Knee pain aggravation ascending stairs. Diagnosed COPD by pulmonologist. Since the improvement was not significant she approached us for homeopathic treatment. Previous Investigations -7/8/19 PFT SEVERE OBSTRUCTIVE RESTRICTED AIR WAY DISEASE. XRC LEFT CONSOLIDATION. S. Uric Acid- 6.8 Vit D3- 20 IgE LEVELS 1234 Rx- Baccilinum 200 1 dose, followed by Natrum Sulph 200 weekly. Acute remedies were used for exacerbations of condition. Gradually along with Inhalers she improved and her inhalers were tapered and were only used if required.
A CASE OF ASTHMA
On 05/01/2018 a 40/F, Mrs. V. A came to us, complaining of breathlessness since September, 2017. There was an episode of Pneumonia after which the complaints had aggravated. Sneezing in the morning on waking up. Tendency to colds and cough which was prolong aggravated into asthma attack .There was involuntary sighing+. Wheezing respiration generally at night. Constant state of stress and fatigue. Worried about children’s health and sleep is disturbed. Allergic colds since 3.5 years. Chilly state. Loves chocolates, sweets, junk food. Can’t take cold air, and usually falls ill. Easily gets exerted and weak. Prefers warm bath. Taking inhalers and steroids for her complaints. Rx : Kali carb 10 M weekly reduced her intensity and gradually totally responded with the remedy.
A CASE OF ALLERGIC SINUSITIS
On 09/05/2020 Mrs. S K, 42/F came to us with complaints of Allergic Sinusitis which started after her pregnancy 6.5 years ago. She complained of severe nose block due to pollen especially in spring. Blocked sensation from nose to the middle of the throat with profuse sticky mucus, which causes difficulty in breathing. It becomes worse in the evening, and better if she is walking in her garden. Head heaviness with occasional vertigo. Sleep disturbed due to suffocative feeling. Sinuses were tender. Thermal state Chilly. Rx : Kali Bichromicum 200 weekly was prescribed as constitutional remedy and Pulsatilla- nigra 200 frequently follow of 6 months relieved her symptoms.
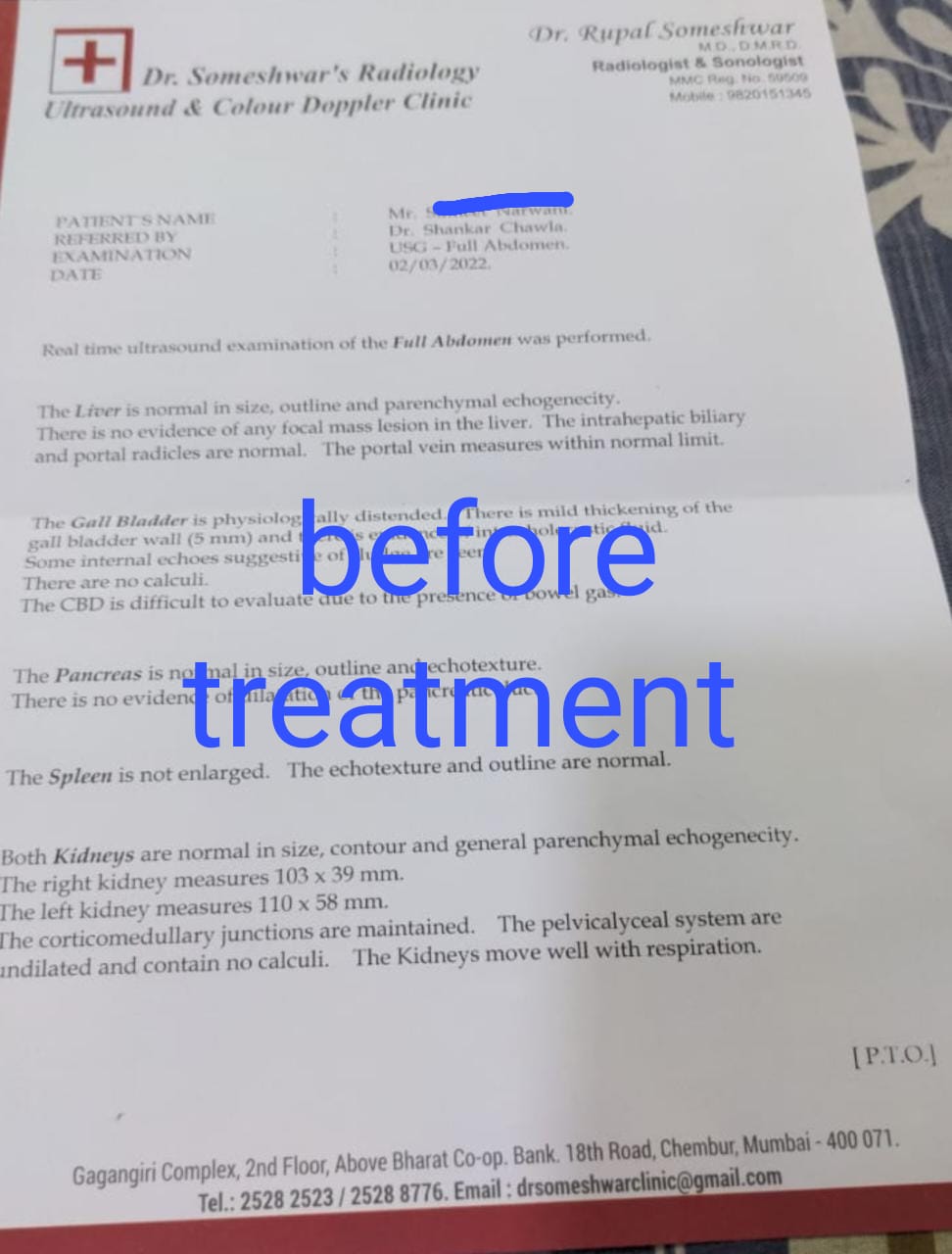
A case of Gall Bladder Acalculous Cholecystitis
Name SKN Male age 33 years presented in acute severe sudden pain in abdomen unable to localise the pain in abdomen on 1/3/2022 around 10.30 pm with a lot of discomfort, restlessness, and distress. The pain was so severe that he sat on the ground pressing his abdomen with both hands. There were also loud empty eructations with no relief. H/o vomiting twice with no relief. Severe pain started half an hour ago. H/o similar pain about 3-4 months back which was mild and subsided on its own. Examination abdomen soft Liver Spleen not palpable no history of any co-morbidity. There was significant weight loss reported since the patient was very uncomfortable and in distress, detailed history could not be elicited. The patient was advise Usg of abdomen and blood investigations Magnesium-Phosphorium 30 potency was prescribed. Usg abdomen dated 2/3/2022 findings were consistent with acalculous cholecystitis. Routine blood investigations, Liver Function Tests, and Lipase Amylase were within normal limits. Based on his constitution, the patient was prescribed Lycopodium 30 3 doses weekly for 3 months. Repeat Usg abdomen on 25/7/2022 compared to previous report changes in the gallbladder have resolved. There was one mild episode of pain which subsided with a few doses of Magnesium Phos 30. There has been no pain reported for 6 months. Acalculous cholecystitis is mostly a surgical condition with high morbidity and complications. The right remedy has the affinity to penetrate and reverse the process in this case.
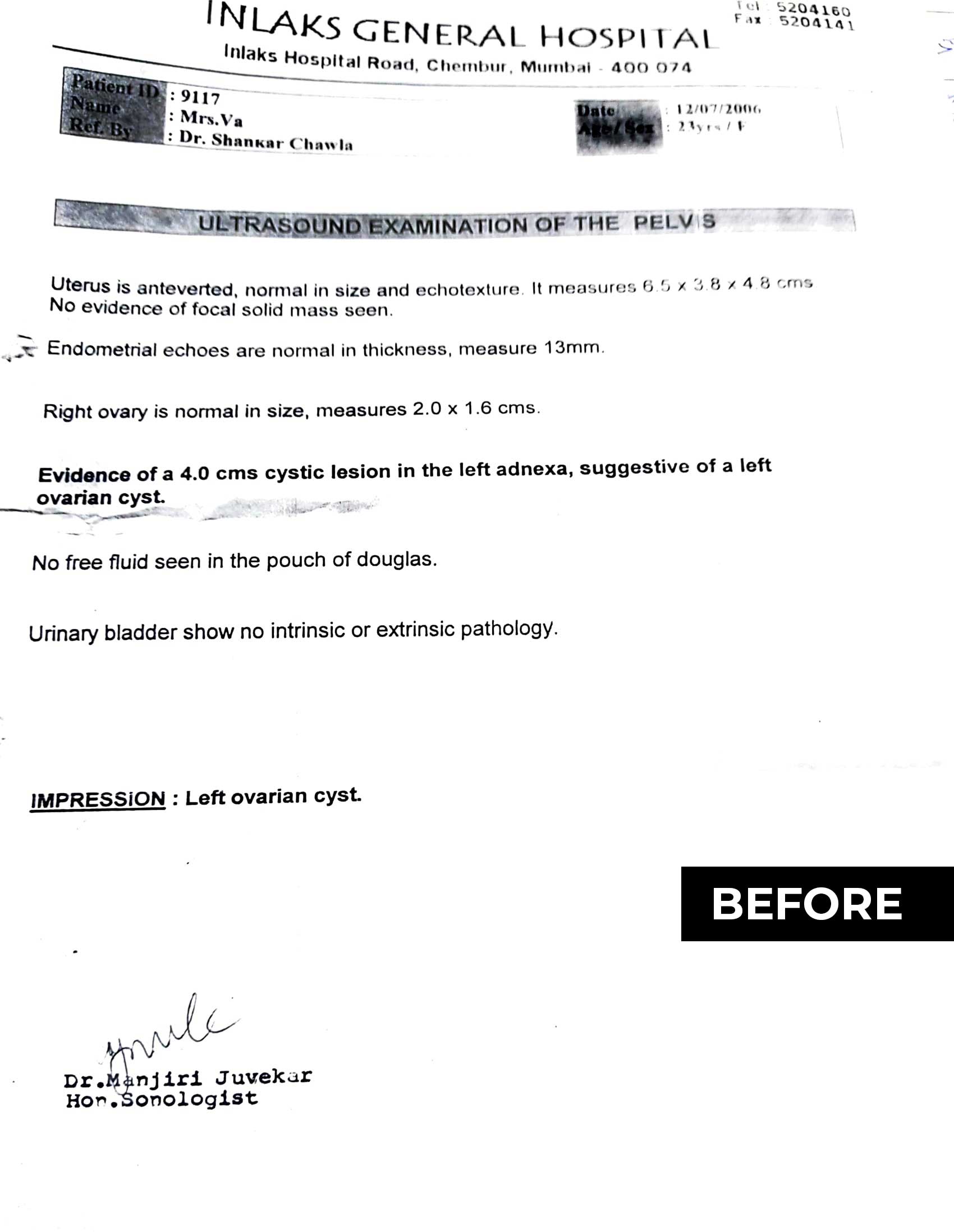
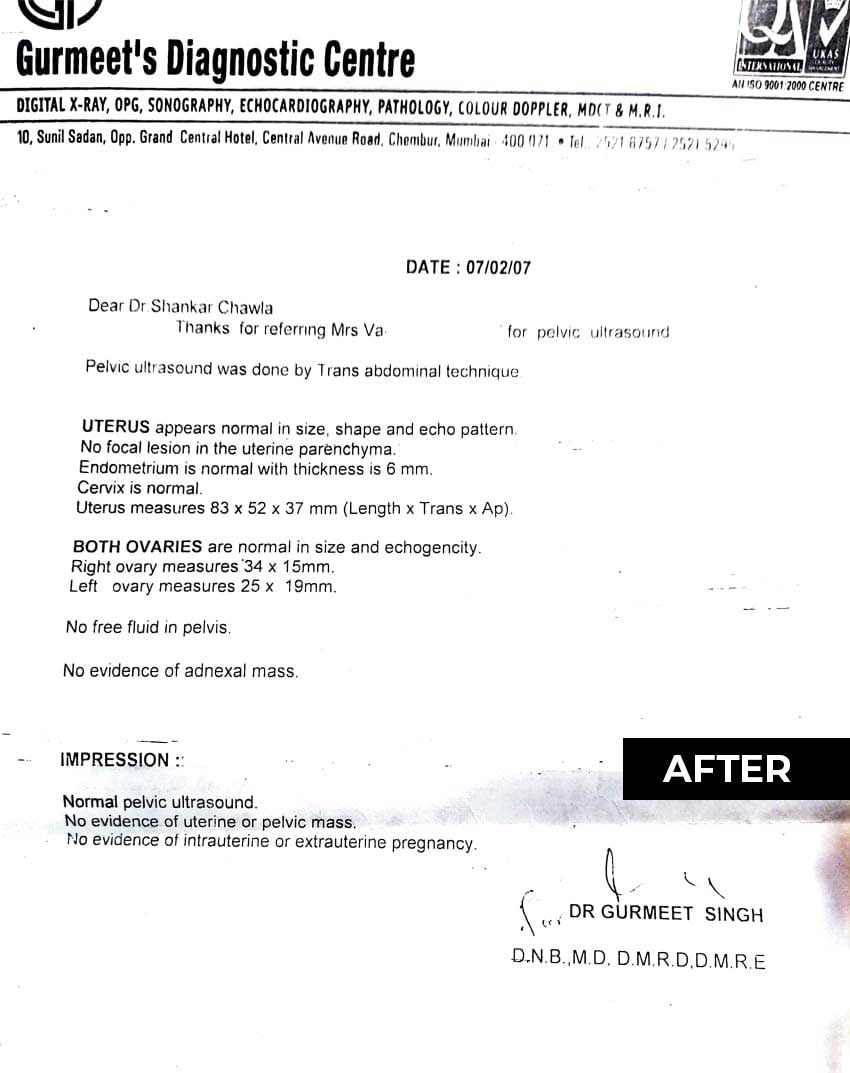
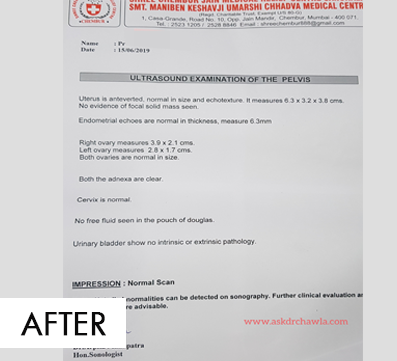
CASE OF PCOS
Mrs. V. G., 23/F, consulted us for her PCOS in May 2006. She had left ovarian cyst measuring 4cms, in the left adnexa. She had irregular menses since January 2005 . There was pain in the abdomen on the first day of menses , and duration was 3- 4 days. Menses were sometimes delayed or the flow would vary. Along with this her associated complaint was cough and cold which was severe. Cough would be thick yellow expectoration agg in the evening. Thirst and Appetite was low, thermally- hot and perspiration moderate on back. On asking about life situation, her nature is mild and weeps easily. We first prescribed her Pulsatilla 200. On the further follow ups, her respiratory complaints were less frequent then. Her old complaint of backache reappeared which was aggravated after exertion. Pain on the first day of menses had reduced. Sleep was disturbed due to backache. Acute complaint of breathlessness started in November 2006, and we prescribed Kali Carb 200. We continued with Kali Carb as her constitutional dose and Pulsatilla in acute pains , colds and cough. By the end of 2006, her menses were quite regular, dysmenorrhea had eased out. In February we repeated the USG Abdomen, which was absolutely normal.
CASE OF TONSILITIS
A 29/F, Ms. S. R. P was complaining of recurrent tonsillitis since the age of 16 years on 11/09/2019. Complaints aggravate every 2 months, on eating anything cold. Throat pain and soreness with no desire to eat or drink due to pain. Chilly patient. Perspiration profuse on head. H/O Swine Flu in 2018 and very strong family History of Asthma. We gave him Tuberculinum ( I dose) followed by Hepar Sulph as sos. He improved well in the next two weeks. The next episode was less severe that the usual ones, so Hepar Sulph was repeated since his sore throat was better by warm liquids. In subsequent follow ups, the recurrence decreased and the intensity of the symptoms also went down.
CASE OF ALLERGIC SINUSITIS
On 09/05/2020 Mrs. S K. , 42/F consulted us for her complaints of Allergic Sinusitis which started after her pregnancy 6.5 years ago. She complained of severe nose block due to pollen especially in spring. Blocked sensation from nose to the middle of the throat with profuse mucus, which causes difficulty in breathing. It becomes worse in the evening, and better if she is walking in her garden. Head heaviness with occasional vertigo. Sleep disturbed due to suffocative feeling. Sinuses were tender. Chilly patient. We prescribed Kali Bichromicum . On 13/06/2020 Blocked sensation > by 40 percent. Head heaviness++
CASE OF ASTHMA
A 40/F, Mrs. V. A came to us, complaining of Asthma since September, 2017. There was an episode of Pneumonia after which the complaints had aggravated. Sneezing in the morning on waking up. Tendency to colds and cough which agg into Asthma attack .There was involuntary sighing+. Wheezing respiration generally at night. Constant state of stress and fatigue. Worried about children’s health and sleep is disturbed. Allergic colds since 3.5 years. Chilly state. Loves chocolates, sweets, junk food. Can’t take cold air, and usually falls ill. Prefers warm bath. Taking inhalers and steroids for her complaints. Kali carb doses weekly. On 23/01/2018. Sleep improved. Sneezing is slightly better. The next follow on 22/03/2018 the Physician had reduced the steroid dosage. Wheezing>> . Morning colds>. Anticipatory anxiety >. So Kali Carb was continued.
P.S – Her panic state made the breathlessness worse, so since the mental state qualifies her physical complaints, we prescribed high doses of the medicine.
CASE OF CHRONIC BRONCHITIS
A 64/M, Mr. C. D., a chronic smoker was complaining of severe breathlessness on sitting and dry cough. On Examination chest had rhonchi++. Recent history of angioplasty in Jan 2019 with severe occlusion in LCX artery. Bloating of the abdomen++. For his acute complaint we gave him Spongia Tosta in frequent doses. The next follow up on 05/08/2019- Cough was better in the past one month but then Cough agg since a week inhalation of fumes. Other associated complaint was Bloating of abdomen and an old complaint of lumbago . Lycopodium was prescribed them as a constitutional. On 19/09/2019 Cough >, with difficult expectoration and Bloating of abdomen+ with flatulence so Lycopodium was continued.
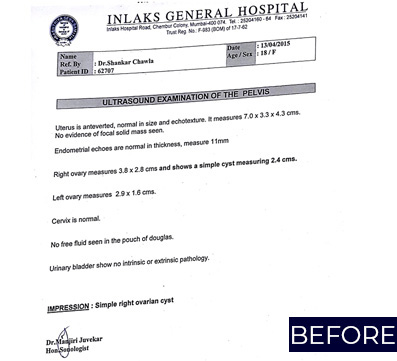
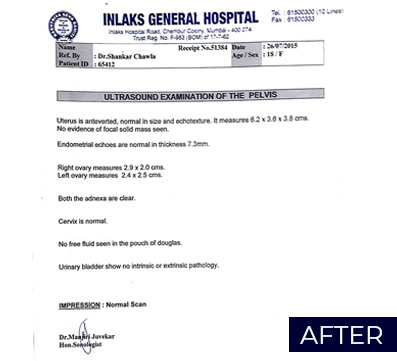
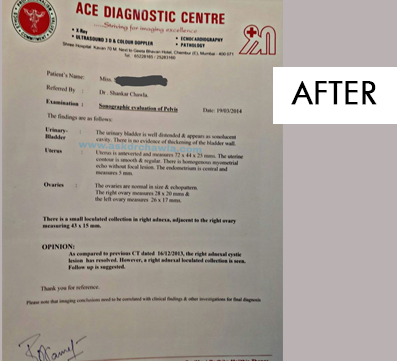
Case of Complex right ovarian cyst.
A 17 year old female, came to the clinic with the complaint of irregular menses since 8 months on 7th October,2014 . There was amenorrhea for the past 4 months. She was advised USG abdomen along with other blood tests. The USG reported suggested of a Complex Right Ovarian cyst and other blood tests were normal. The patient was advised surgery for which she was reluctant and wanted to try Homeopathy. She was of nervous temperament, the anxious feeling would increase before exams. Her associated complaint was of hair fall. She was given Pulsatilla according to her current state keeping in mind all the generals and particulars. The menses came on 22nd October, 2014 for 8 days. The hair fall reduced considerably within 3 months. There was an episode of menorrhagia in February 2015, which lasted for 9 days. Her anxiety was also controlled. On 13th April, 2015, USG was repeated and it suggested Simple Right Ovarian Cyst. But the other blood tests indicated that Testosterone levels were high and Vitamin B12 levels were low. There was only one cycle which was irregular later on and then the menses were regularized. On 26th July, 2015 the USG was repeated and it was completely normal along with all other blood tests.
Note- Calcarea Phosphoricum was administered along the course of treatment as per the indications.
Case of Chronic Migraine
A 29 year old male came to us on 26th February 2019, with complaints of Chronic Migraine since 8 years, Pain in the occiput and left side of the head which would aggravate in the evening, sensation as if head is vibrating. Headache would aggravate in sun. Pain in the cervical region along with the headache. Life situation indicates there is business stress. On asking further about mental and emotional state, he mentioned about his grief about losing his mother and brother 9 years ago. His mother passed away due to sudden Myocardial Infarction and brother in a road accident, within a year. He started having sleepless nights and appetite reduced. Dreams are frightful of dead people. He was given Ignatia Amara (1 dose). Follow up on April 02, 2019 suggested his pains improved, sleep is still disturbed with the thoughts of his mother. He was given Natrum Muriaticum (1 dose). By July , 2019, patient mentioned said that there have been no episodes of headache since the past one month. The sleep was much better, and there are no frightful dreams now.
P.S- Belladona was given as an acute for his pains.
Case of Alopecia Areata
An obese 25 year old female, came to our clinic in July 2019 with complaint of severe alopecia. There is baldness of scalp, thinning of hair with hairfall. She is known case of Hypothyroid with raised with TSH (5.7) and PCOS since many years. The complaints of hair fall started with chemical bath in the sea?. Mother says she gets angry easily, but cannot express her emotions. Menses are regular with pain in the back and abdomen during menses. Perspiration is moderate in axilla and scalp. She is a chilly patient and complaints headache on exposure to sun. She has aversion to sweets as well as bitter. Academically she was quite poor in childhood. She was given BarytaCarbonicum (doses). On July, 12 she said her hair fall is reduced. She had heel pain in the morning on waking up. The doses was continued. Follow up of September, 2019 showed stagnation in recovery, anti-miasmatic dose was administered- Thyroidinum (1 dose). In January 2020, the TSH values reduced to 5.1. The bald patch has improved considerably. The heel pain is diminished. The hair thinning has also reduced. The patient still under our treatment.
Case of Adenocarcinoma of the Head of Pancreas for palliative treatment with Homeopathy.
On 12th July, 2018, a 73 year old male, came to the clinic diagnosed with Adenocarcinoma of Stomach and duodenum in 2015 which had progressed to the head of Pancreas. The medical history of the patient suggested that Ejection Fraction of the heart was 15%, had lost 6kgs in 45 days, and the Serum Creatinine had been fluctuating between 3.5 and 2.5 since June. The serum electrolytes values were low and Hemoglobin was 9.7. Post CABG surgery in 2005, he had developed complete blockage in one artery and 95% blockage in two other arteries. Since the disease was at an advanced, progressive and eventually fatal stage, he was advised for home care by the Oncosurgeon. With this awareness of the outcome and the weakness the patient was also not willing to go for chemotherapy or surgery. Adenocarcinoma – originates from glandular tissues or structures. Pancreatic cancer is fatal and the prognosis is very poor. The survival period varies from 6 months to 3 and half years. This case demonstrates role of homeopathy in palliative care in Cancer. He complained of severe abdomen pain with weakness. The patient had episodes of vomiting- greenish discharge and Phosphorous was given repeatedly for couple of weeks. On 26th July, in the follow up the Patient had been feeling better. After a month he complained of burning sensation in the abdomen with persistent pain and Arsenic Album was given. Colocnyth and Iris Versicolor was prescribed as SOS for pains as per the indications during the course of treatment. In palliative cases, the remedy keeps changing as the phase/state changes. In such cases the focus is to reduce the journey of suffering mentally and physically and to improve the quality of life. The last follow up was on September 06, 2018 for his pains and complaint of fissures, was given Capsicum. The patient passed away peacefully in sleep at home in October, 2018. P.S- The remedies prescribed in such gross pathological cases are in low potencies.
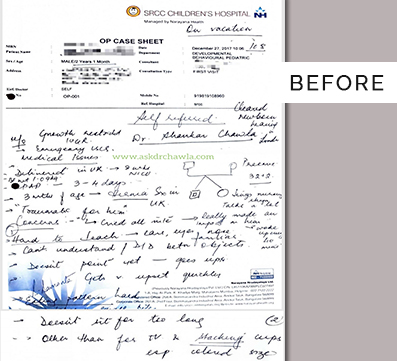
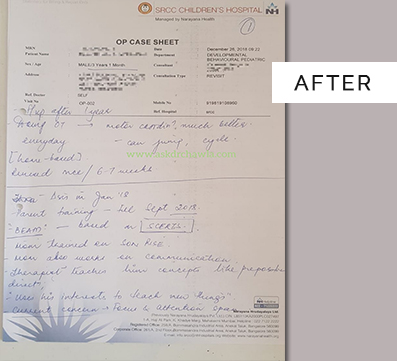
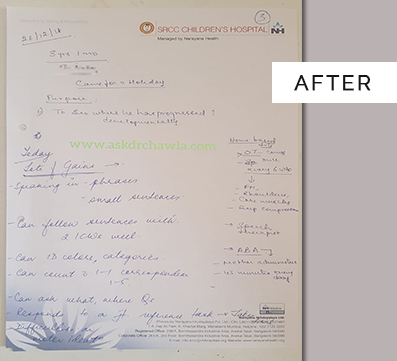
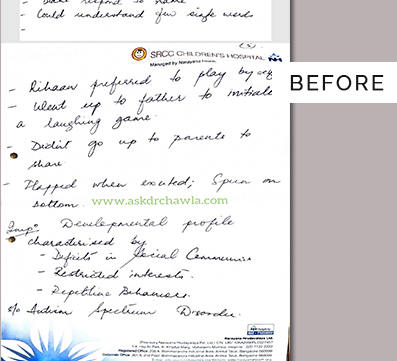
Case of Autism
Mst. R. A, one of the twins, 2 years and 1 month old, was referred to us on 3.12.2017. The mother complained of Behavioral Problems. The opinion of a Pediatric Neurologist was taken and was diagnosed as Autism. The child was an IUGR baby. Mother said he was very stubborn, clenched his teeth in anger, and shouted in excitement. He would get attached to the person who has slept him with that night and demands attention from that person the next day. He would cry for attention until given. His speech was unclear and would not be able to concentrate when taught something or pay any attention. He would throw his toys and food in anger. He also has recurrent cold and cough leading to severe respiratory distress that he requires inhaler- 8 to 10 puffs every 4-5 hours. The congestion and phlegm is better by vomiting. Wants to be carried around and wants to be touched all the time. The child has chronic constipation with offensive stools and flatulence. One very important characteristic of the child was , he did not like enclosed surroundings, he would not like to sleep in the cot and wouldn't allow to put the seat belt across. He was given Spongia 30 repeatedly for the first week for the cough and Calcarea Carbonicum (1 dose) was administered. In January, the complaints improved and the number of inhaler puffs were reduced to 3-4 / day. Over the span of next 10 months, there were acute episodes of fever and cold but the frequency and intensity had reduced marginally. With every follow up his complaints of constipation decreased and changes in behaviour was seen. In December 2018, the patient was seen by the Peaediatric Neurologist again as a follow up and she mentioned that the child is now near normal. P.S- Other acute remedies like Arsenic Album, Antimony Tart and Merc Sol were given as and when required.
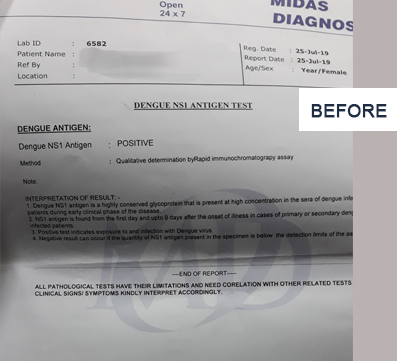
Case of Dengue
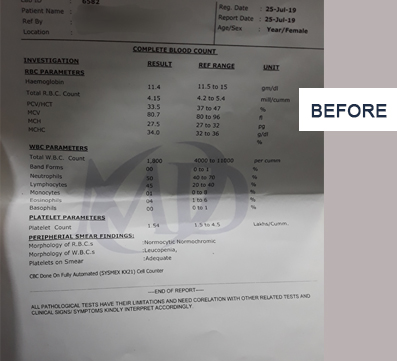
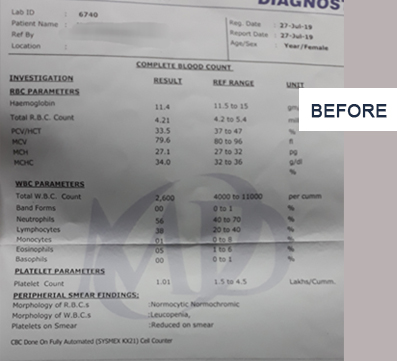
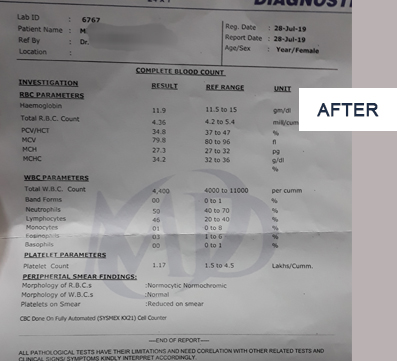
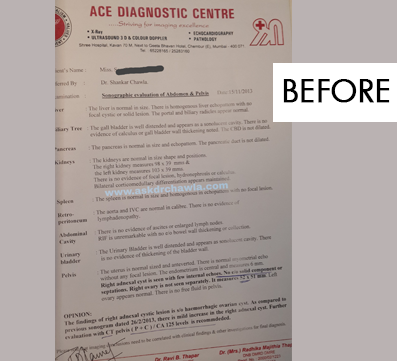
22 year old Ms. Y. P., came to the clinic suffering from severe depression on 26/06/2019. She said that after a wearisome and tedious admission process for her academics she started developing anxiety. And then it lingered on and then she started showing signs of depression over a period of 18 months because of work and education pressure. She has been on anti- psychotic medications for about 9 months. And now has been tapering the dosages. She has been having frequent headaches. On 09/07/2019 after evaluating the entire case history and analysis, constitutional dose – Calcarea Carbonicum (1 dose) was administered. After a week the intensity of headache had increased so Gelsemium (3 doses) were given sos. On 25/07/2019 the patient came with an onset of fever with headache and prostration since 3 days and Arsenic Album 200, 5 doses were given. Investigations were advised and results were- HB- 11.4, WBC- 1800, RBC- 4.15 PLT- 1.54, and POSITIVE NS1 (DENGUE) TEST. On 27-07-19, The patient was sleepless, with increasing pain in the lower limbs, thus Eupatorium Perforatum 200 (3 doses) were given and the investigations were repeated- HB- 11.9, RBC-4.36, WBC- 4400, Platelets- 1.17. On 29/07/2019 the patient came back again with a characteristic complaint of Itching during spikes of fever. One dose of Kali Brom 1M was given immediately, and few doses as SOS. Patient called again after 4 days saying she was completely better.
Case of Gangrene
Mr. S. G. , 65 year old, known case of OA(knee joint), Diabetes Mellitus and Gangrene, walked to our clinic with a lot pain in his lower extremities and swelling, on 22.06.2013. History of chewing tobacco and drinking alcohol since many years. He runs a small shop in the village since he was 10 years old. He complaints of pain and stiffness in the knees while walking. Past history of surgical intervention of hemorrhoids - 12 years ago. He desires non-vegetarian food. The patient said the he gets angry easily and sometimes shouts too. Other generals were normal. The right feet was affected with gangrene, the extent was from instep to right lateral malleolus to the sole of the feet. It was black discoloration with irregular margins, and discharging with thick gelatinous fluid. SECALE COR 30 was given repeatedly for the first two weeks. On 03.08.2019 Kali Bichrom 200 (1 dose) was introduced as the constitutional medicine. By 21.10.2013, revascularization and granulation tissue of the affected area was seen. There were no discharges from the wound and the swelling had reduced considerably, knee pains had improved too. The follow up of 14.12.2013 showed skin regeneration and healing.
Case of Hemorrhagic cyst
On 8th November, a 27 year old female, Ms. P.S., came to the clinic, with past history of Typhoid (2008) and TB Lung (2001) and currently complaining of pain in the right abdomen , dull type, constantly. Her menses have been irregular since few cycles. The USG reports dated February 2013 suggested Right ovarian adnexal mass s/o Hemorrhagic Cyst measuring 40mm x 30mm. We advised one more ultrasonography to understand the current situation and extent of the lesion. USG done on 15th November 2013 reported increase in the size of the lesion to 50mm x 51mm. Pain radiated from right abdomen to the thigh. She also complained of bleeding hemorrhoids as well as backache which had been a chronic. Associated complaints were physiological leucorrhoea- sticky, yellow and offensive, 15days after that would cause itching and burning in the vulva. Generalities- hot patient, thirstless and moderate sweat. In her life space she mentioned that she gets irritated very easily, weeps alone and like consolation, feels like she is losing interest towards evening and difficulty in concentration. Considering her chief complaints, physical and mental situations the symptoms were evaluated and THUJA (1 dose) followed by KALI CARB (1 dose) in the following week was administered. MAGNESIUM PHOSPHORICA was given as SOS for her pains. We administered ARSENIC ALBUM few doses for her acute complaints of ineffectual urge to pass stools, colds after taking cold things and constant desire to itch with burning in the genitals. After about 1 month the other complaints started settling, but abdominal pain remained the same. PULSATILLA (1 dose) followed by ARSENIC ALBUM (1 dose) was given in the following week. After 2 weeks the pains and itching had increased, NATRUM MUR 200 (1 dose) had been given. The pains and itching had slightly reduced in the next follow up. But the abdominal pains continued and even the boils, PULSATILLA (2 doses) were given in higher potencies.
Note- In Chronic cases, there is no single remedy which can take care of all the complaints. As when the picture gets clearer, and the state of patient changes, the potencies of the remedies have to be changed as well as there may be a need to change the prescription. All this is considered by the physician and after keen evaluation the prescriptions are made. IN THE ABOVE CASE, PULSATILLA HELPED THE MOST. BUT OTHER REMEDIES ALSO PLAYED A CRUCIAL ROLE.
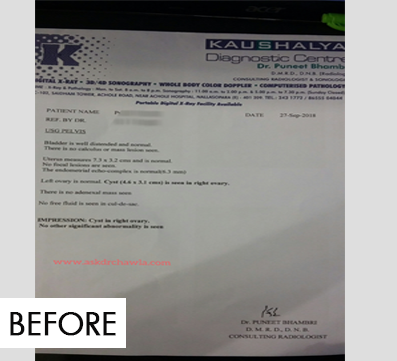
Case of Ovarian Cyst
A 28 year old female, Mrs. P. G. Visited us on 2nd October 2018 with her sonography reports suggestive of right ovarian cyst measuring 4.6 x 3.1cms. The uterus as well as left ovary measured normal. Gynecological history suggested that she had been having irregular menses since the past few months and cycle was of 45-50 days which earlier was of 30 days. Her L.M.P was- 24th September, 2018 and menses lasted for 7 days, bright red bleeding with clots and leg pains after menses. While taking the history there was strong discontentment that she felt with her family and the surroundings. As her constitutional we administered Calcarea Phosphoricum (1 dose), followed by Thuja (3 doses) in the following week for few weeks. In her next follow on 16th November, L.M.P- 23rd October 2018, the duration of menses as well as the flow had reduced in this cycle. In the subsequent cycles the pains also reduced considerably. Pulsatilla (2 doses) was administered when the menses were late in couple of cycles. By April 2019, her cycles had regularized, clots had decreased considerably and even the leg pains. After monitoring her cycles, sonography was repeated which was completely normal without any ovarian cyst.
NOTE- THE ABOVE REMEDIES WERE PRSECRIBED AFTER EXTENSIVE CASE TAKING AND EVALUATION OF THIS PATIENT. OUR TREATMENTS ARE BASED ON OUR UNDERSTANDING AND EXPERIENCE.
Case of Psoriasis
A 56-year old retired female, came to the clinic on 19th Jan’ 16, with her chronic skin complaints – - of PSORIAIS that she had been suffering from past 10 years. She used to work in a hospital as a helper. The onset of eruptions were from the lower extremities – left foot and then spread all over the body. The eruptions are painful, itchy and oozing with offensive discharge. There was burning sensation in the eruptions all over the body which would aggravate at night along with itching. She was a K/C/O of HTN and SLE. PSORIASIS. The skin turned hyper pigmented and black. When asked about her life situation and current state of mind we learnt that she currently stays alone and has to take care of her own self, husband had passed away few years ago. She was quite anxious about her health (which was considered an important characteristic in evaluation), fastidious and critical about others. Chilly patient, thermally, but sun would aggravate her skin complaints. Investigations done on 30th Jan, suggested : Hb- 9.5 , N- 20.7, E- 18.4, S. Uric Acid- 10.7 , E.S.R.- 113 , IgE - 320, Lipids : TGL- 200. After analysis and evaluation of this case, Arsenic Album 200, two doses were administered initially and positive results were seen. At the end of four months, the above investigations were repeated, and they were normal. There were no new eruptions, no itching and change in skin colour within 8 months.
NOTE- The remedy chosen was based on the characteristic symptoms present in this case, it is important to know that is every psoriasis case will not be better by Arsenic Album.
Case of Bullous Pemphigoid:
On the 5th of March'18, a 4-month-old baby S., was brought to us by her mother with the complaint of blisters and pustular eruptions spread extensively on the body. Redness and swelling of the feet and hands were seen. On examination, diagnosis made was as Bullous Pemphigoid. The complaints had started in last month of 2018. The eruptions appeared as small vesicles on the abdomen, back, upper and lower extremities and then extended to the scalp. She was admitted in the hospital for 3 days for her acute respiratory complaints, after which the skin complaints had slightly reduced and then reappeared severely. It progressed as pustular eruptions from the webs of toes and feet to the hands. The nails were discoloured. Mother's history during pregnancy revealed that she had Gestational Diabetes and was on the medications throughout her pregnancy. She also mentioned that she was under a lot of stress due to family issues with her in-laws. The father worked on the ship, so he was seldom around. The patient's generals were normal. Dulcamara 200, 2 doses were given in a week. Later on, as the case and complaints evolved further on 12th March'19, Merc Sol 30 (1 dose) was given for her itching and increase in the number of pustular eruptions on the scalp. She responded very well within 2 weeks, the eruptions started drying and size of the blisters started reducing, no new eruptions or blisters were seen and the itching had reduced considerably. It was then repeated infrequently as SOS. An intercurrent was introduced to boost her immunity, and so that the complaint does not linger for long and symptoms do not reappear. After which the eruptions disappeared completely. In the last follow up there was no redness, itching or any new eruptions in 2 months.
Case of Delayed Milestones:
A case of child P.: A 31/2 year male child came to me on 21.03.2001 with mother complaining that he is not speaking. On observation this child had good eye contact and was very hyperactive would not sit in one place. He would frequently go to mother and kiss. He was shy, timid would hide behind the chair or mother and fearful look would give a smile. He had the tendency to recurrent cough and cold. He was examined by paediatrician and could not find any abnormality and labelled as delayed miles stones and recommended speech therapy. His mother is a teacher in M.P and they stay in Chembur Mumbai as father is a contractor. She has taken a prolong leave but has to report often to attend school for period. Pinto used to feel insecure without mother. In view of other characteristic feature he was prescribed Agaricus 200 in infrequent doses. He responded very well in terms of speech. We really found difficulty in school as he was unable to cope up, a time came that the school recommended a special school for him. Remedies such as Stramonium 1M was given for fear, Calcacrea-Carbonica 200 was introduced for his constitutional dose. He was able to cope and is going to main stream school of class IV and is performing well in his studies. Mother being the teacher was a good source of help in making him study.
A young studious girl studying in X std class, age 15 years name S. came to me for lack of concentration, forgetfulness, unable to focus for long, easily distracted. She looked tired, fatigue, dull with drooping of eye lids. Mother described that she is exerting mentally because of her studies and is stressed out. On further questioning she said that she feels nervousness, trembling before her exams and has heaviness of head. In spite of studying and knowing the subject she was not confident. Her performance had been low because of these conditions. She was given Gelsemium samperverus 1m and Kali phosphoricum 200x 4 pills twice a day for 2 weeks. She was able to perform well and her nervousness had reduced which did not interfere with her performance.
A case of Ovarian Cyst: A female age 35 years Mrs C. working as a typist, came to visit our clinic on 24.04.2000 with complaints of pain in abdomen colicky in nature with history of vomiting unable to retain for 2-3 days. Her Usg on 11.04.2000 shows large thick an echoic pelvic-abdominal mass (with clear fluid)? Left T.O. mass. On examination, per abdomen a lump extending up to epigastrium region. Her menses were very painful heavy for 2 days and were regular. Her general examination WNL. Her mental state reveal emotional suppression were her In-laws were causing her trouble in day to day chores. She craved spicy++, sweets+ in food, sun causes headache. She was given a dose of Natrum- Muraticum 200, she developed increased pain after 2 days of dose which subsided in few hours. Repeated Usg done on 11.08.2000 shows considerable regression in the size of the left T.O.Mass. Latest Usg shows total regression of mass.
A middle aged obese man A. G. aged 36 years a known case of Irritable Bowel Syndrome came to us on 20.04.2007 with symptoms of distension of abdomen, bloating, eructation, constipation occasionally most of the times diarrhoea loose stool 2-3 -5 times a day after eating, drinking since 10 years. All investigation done including sigmiodoscopy showed normal. His occupation initially working with shares and mutual funds Company with sedentary lifestyle and off late started his own business. He was always on edge with his work to complete the targets and felt very frustrated because of his work. He desires spicy, fried which aggravated his condition with his irregular eating and sleeping habits his life had become miserable and on top his business in today's time of recession was at low. We prescribed him Nux-Vomica 1m daily dose with weekly dose of Dys-co1m. His response to treatment was satisfactory but his general low energy levels and residual gastric symptoms persisted. His stress level also remained same. He wanted to try Acupuncture, with 15 sitting he dramatically improved. Acupuncture brought back his energy, improved his sexual performance and was able to cope with his occupational stresses and also started his own business.
A case of Elderly man Shri C.G. age 76 years came to us on 23.06.06 with diagnosis of early Parkinsonism, Benign enlargement of prostate, retinal detachment, gall stone, on hypertensive medicines. C/o trembling+, shaking+ of upper limb, loss of memory, chronic mucus in stool with unsatisfactory stools. He was fully investigated and seen by all the experts and consultants. With all this he was living a very active life till the wife was alive. Her wife suddenly died on 13.03.2006. All his condition started deteriorating. It times becomes very difficult to understand the mental state especially in cases were maze of symptoms present and there is a compensated state. He presented very bold, strong and did not reveal any emotional weakness in few follow-up. Once the rapport was developed he said that he no longer what to live as he wife has left her he feels lonely, sad, depressed and unable to sleep. He was well looked after by their children and daughter in laws and was respected by family and society. His family and friends were concern about his deterioration of health. He was undergoing a grief we prescribed him Ignatia amara 1m followed by Natrum-Muraticum1m and he also required a dose of Aurum-Metallium 1m. Elderly man is a changed man now, he started work and become active again. He devoted his time for society work. He improved with his LFT, and his gall stone had disappeared in his USG which even radiologist was amazed.